Eating Disorder Awareness Week, 2024
In the United Kingdom, it is estimated that over 1.25 million people are affected by some kind of eating disorder, with anorexia nervosa, bulimia nervosa, and binge-eating disorder being the most commonly diagnosed.
However, this year, Eating Disorder Awareness Week is dedicated to a lesser known disorder called avoidant/restrictive food intake disorder (AFRID), which accounts for approximately 5% of eating disorder cases in the UK.
So, what is avoidant/restrictive food intake disorder (AFRID)?
The term avoidant/restrictive food intake disorder (AFRID) has only been around for the last decade or so, and so, it's understandable that many are still unaware the diagnosis exists. In fact, AFRID used to be known as ‘selective eating disorder’, but diagnosis’ were very rarely handed out, and often those with AFRID were just reduced to being categorised as ‘fussy’ or ‘picky’ eaters.
However, since 2013, AFRID has been a recognised mental health condition that is characterised by a pattern of avoiding certain foods, or food groups, and restricting the amount, or types, of food that is consumed. People with AFRID tend to stick to the same meals and snacks, which, if left untreated, can cause nutritional deficiencies or more serious health concerns later down the line.
And, what causes AFRID?
Unlike a lot of other eating disorders, body image issues or concerns are not the most common reason AFRID develops.
In some cases, a person may just not recognise their hunger and have a poor appetite, or they may not enjoy the physical act of eating so it feels like a chore, causing a low interest in eating, and unhealthy eating patterns. But for most, the reason behind their avoidant/restrictive food intake disorder is rooted in their senses and/or memories.
Depending on the individual, a certain food type may be avoided due to a sensory reaction to the taste, texture, smell, or appearance of certain foods, or, due to a memory-induced reaction, that is triggered by an unpleasant memory of eating that food, which now causes the mind to be avoidant of that food altogether.
Eating disorders in the UK
Categorised as mental health conditions, eating disorders cause a person to use food as a way to cope with, or control, their emotions and/or experiences. The three most common types of eating disorders in the UK, are anorexia nervosa, bulimia nervosa, and binge-eating disorder.
What is anorexia nervosa?
Often shortened to the term ‘anorexia’, anorexia nervosa accounts for around 10% of eating disorders in the UK. People with anorexia typically have very complex relationships with food, and take, what some would see as drastic steps, to avoid eating and/or keep their weight down.
Common behaviours, and signs of anorexia nervosa include:
- Counting calorie intake closely or obsessively (often consuming far lower than the recommended 2,000kcals+ a day)
- Avoid eating foods that are fattening
- Skipping meals
- Eating very small portions
- Engaging in excessive levels of exercise
- Having a low BMI
- Taking appetite suppressants, laxatives and/or diuretics
What is bulimia nervosa?
According to the Priory Group, around 40% of those with an eating disorder have bulimia nervosa or ‘bulimia’. Unlike those with anorexia, who tend to avoid foods when and where they can, people with bulimia typically eat a large amount of food very quickly to get the satisfaction from tasting and eating food, but then quickly purge what they have eaten in an attempt to stop weight gain.
Common behaviours and signs of bulimia include:
- Episodes of uncontrolled over-eating or binge-eating.
- Hiding foods, or having a ‘binge stash’.
- Frequent visits to the bathroom
- Self-induced vomiting
- Use of laxatives
- Preoccupation with body image
- Poor dental health
What is binge-eating disorder?
Binge-eating disorder, or BED, is experienced by around 1 in 50 people in the UK. When a person has binge-eating disorder they regularly over-eat, or eat a large volume of food in a short period of time which causes them to feel uncomfortably full or bloated. Sometimes these binge-eating episodes are planned, and sometimes they occur spontaneously, but they are often accompanied by feelings of shame, depression, or guilt.
Common behaviours and signs of binge-eating disorder are:
- Eating very quickly during a ‘binge’
- Eating past the point of satisfaction
- Eating when they are not hungry
- Eating in response to emotional stress
- Secretly eating, or wanting to eat alone
- Sensing a lack of control when it comes to eating
- Obsessive thinking about food or experiencing strong cravings for certain foods
Treating eating disorders
Usually, eating disorders develop during childhood or adolescence, and tend to affect people most intensely during this period of their lives. While eating disorder recovery is tough, it is possible, and there are many different approaches (and time frames) involved in treating eating disorders, because they are unique to the individual.
In the UK, typically supervised weight gain and talking therapies are the first recommended route of treatment for eating disorders. This may involve sticking to a realistic and achievable meal plan, working with nutritional support, or undertaking cognitive behavioural therapy, specialist supportive clinical management (SSCM), or focal psychodynamic therapy.
Co-morbidity is also high amongst those with eating disorders, and they are regularly accompanied by other mental health disorders like anxiety, depression, and/or obsessive compulsive disorder. These conditions can intensify eating disorders and their triggers, and so, people with eating disorders may be offered antidepressants or SSRIs as an adjunctive treatment.
Unfortunately, for some, these treatments and therapies don’t successfully manage all their needs, or they experience unpleasant and unwanted side effects from their prescribed medicine, and they are unable to make a full recovery using these options. But, what many don’t know is, they may be eligible for medical cannabis.
Eating disorders and medical cannabis
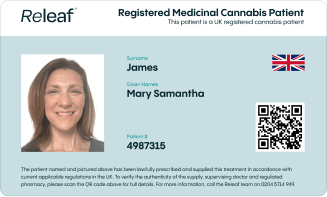
Medical cannabis was legalised in the UK in November 2018 for a wide range of health conditions where other conventional, licensed treatment options have failed. In order to be considered eligible for medical cannabis with Releaf, people with an eating disorder have to have tried at least two conventional treatments that have been unsuccessful in managing their needs, and pass the medical suitability check.
How does medical cannabis work?
Our bodies are incredibly intricate, and there are a number of sophisticated and complex networks and systems that operate ‘behind the scenes’ or under the surface to keep us healthy. One of these systems is called the endocannabinoid system (ECS), which is responsible for ensuring there is balance and homeostasis in the body.
The ECS does this by sending endocannabinoids (chemical messengers) to a specific part of the body, so they can bind to a receptor and initiate a specific response. The endocannabinoid system has receptors all over the brain and body, and is therefore able to influence many biological functions, including emotions and memory, eating and metabolism, pain and inflammatory responses, and so much more.
Cannabis contains hundreds of chemicals, some of which are cannabinoids like THC and CBD. Because they are similar in structure, when cannabinoids like THC and CBD enter the body, they are typically mistaken for the endocannabinoids we naturally produce- and they are able to gain entry to the endocannabinoid system.
From inside the ECS, cannabinoids like THC and CBD can target these different receptors and influence the responses they would typically create. In people with eating disorders, this could mean boosting the sensation of hunger, to increase their appetite, or relieving their anxiety so that mealtimes become less stressful.
Medical cannabis and appetite
The relationship between cannabis and appetite has been anecdotally noted for millennia, but during the HIV/AIDS crisis during the 1980s and 90s a new, and unlikely, advocate for the compassionate use of cannabis emerged.
San Francisco General Hospital’s ‘volunteer of the year’, Mary Rathbun, now known affectionately as Brownie Mary, faced multiple arrests during her late 50’s and early 60’s for baking and distributing homemade cannabis edibles to her patients and friends who were suffering from wasting syndrome.
She did this because cannabis’ psychoactive component, THC, or delta-9-tetrahydrocannbinol, can act as an appetite stimulant.
Upon entering the body, THC can bind to endocannabinoid receptors in our brains, particularly in the hypothalamus (which is responsible for controlling food intake), and can essentially ‘switch on’ the sensation of hunger, which causes an increased appetite - also known as ‘the munchies’.
This may be extremely beneficial for patients who are in recovery from eating disorders that caused them to avoid eating or have a decreased appetite, like anorexia or AFRID, and if used as an adjunctive treatment with talking therapies, with the ultimate goal of weight gain or preventing malnutrition.
Medical cannabis and anxiety
As well as it’s many other responsibilities, the endocannabinoid system is also involved in regulating the reward and pleasure responses or signals that are typically triggered by food intake. In those without eating disorders, this system works ‘normally’ - however, in those who have developed mental health issues surrounding food this system is often considered ‘dysregulated’.
Through its interaction with the ECS, it's believed medical cannabis may be able to ‘normalise’ these responses, and reinstate the pleasure that is typically associated with eating by lowering inhibitions and anxieties - which can make eating less stressful.
THC’s cannabinoid counterpart, cannabidiol, or CBD, is a non-psychoactive cannabis compound that has proven to be effective in relieving stress and anxiety responses - especially in overwhelming situations that trigger feelings of panic or extreme worry.
This could prove particularly useful for those with eating disorders triggered by emotional stress, whether that's refraining from eating when they’re overwhelmed, or if overeat as a way to cope.
Challenges and considerations
With stories like Brownie Mary’s held firmly in the heart of many medical cannabis advocates, and overwhelming anecdotal reports of cannabis increasing appetite, or setting off ‘the munchies’, it is unfortunate that there is such a lack of clinical evidence or scientific exploration into the relationship between cannabis and appetite, and/or eating disorders.
While there is some data and evidence supporting the use of medical cannabis for eating disorder treatment, the majority of this comes from animal studies and self-reported patient surveys as opposed to gold standard randomised, controlled trials which often spearhead treatments into NHS circulation.
Because of this, for now, medical cannabis is not available on NHS prescription to patients who are trying to manage their eating disorder - but these prescriptions are available for eligible patients from private medical cannabis clinics like Releaf.
It is important that the use of medical cannabis is closely supervised by a qualified healthcare professional, like the GMC registered specialist consultants that work for us, to ensure it is providing the best possible results. To find out if these options could be right for you, fill out our free medical cannabis eligibility checker.