Cannabinoids come in two separate groups. First up, we have our own endocannabinoids, which are created naturally in the body. These endocannabinoids act as neurotransmitter chemical messengers in the endocannabinoid system (ECS), sending signals to the ECs receptors (CB1 and CB2) located throughout the entire human body, including the nervous system. Endocannabinoids are fascinating molecules that play a crucial role in regulating various physiological processes, such as pain sensation, mood, appetite, and immune function.
And then we have phytocannabinoids, which are derived from plants, with the cannabis sativa L. genus producing the best known of these, namely Tetrahydrocannabinol (THC) and Cannabidiol (CBD). While both of these cannabinoids have potential medicinal benefits
Understanding the intricate mechanisms of cannabinoids and their interactions with the body is an exciting area of scientific exploration, opening up new possibilities for medical treatments and wellness solutions. There is a growing body of evidence showing that both CBD and THC may very well play an important role in the treatment of pain.
In today's article, we will dig into the currently available scientific evidence on cannabinoids for effective pain management and try to lay out, in simple and easy-to-understand terms, what it all means for those looking to access CBMPs for pain relief.
Understanding the mechanisms of medicinal cannabinoids
To properly explain cannabinoids and the effects they can exert on the body – particularly when it comes to pain relief – it helps to fully understand how they interact with the endocannabinoid system.
Only discovered in 1988, the ECS is now believed to be the 'master' regulatory system of the human body, controlling and regulating a wide range of physiological and psychological processes. These include pain sensation, mood, appetite, sleep cycle, sexual function, inflammation, and immune responses to name just a few.
Phytocannabinoids are able to also bind with these receptors due to their remarkably similar chemical makeup and structure when compared to endocannabinoids. This binding action then triggers a series of reactions throughout the body, resulting in various responses – such as those associated with pain relief.
The main difference between the endocannabinoids and phytocannabinoids lies in how they interact with CB receptors. Endocannabinoids bind very loosely to the receptor, resulting in a short-lived reaction. On the other hand, certain phytocannabinoids (most notably THC) provide more of an 'anchor' on CB receptors due to their stronger binding ability. This means that the response to the binding will typically last much longer.
Understanding Pain
Pain can manifest in three primary forms: acute, chronic, and neuropathic.
- Acute pain is the most common type, typically resulting from injuries like sprains, strains, or post-operative issues. It usually lasts for a few days or weeks before gradually easing.
- Chronic pain is any persistent and enduring pain that lasts for months or even years. It is often associated with chronic health conditions such as arthritis, fibromyalgia, or chronic back pain.
- Neuropathic pain (or nerve pain) is typically described as a burning or electric shock-like sensation and can be caused by conditions such as diabetes, shingles, stroke, multiple sclerosis (MS), spinal cord injury, or chemotherapy. The nervous system itself sustains damage, resulting in the over-excitation of nerves, which produces painful sensations.
THC and pain relief
Now that we have a better general understanding of cannabinoids and how they are able to interact with the body, it's time to dig into THC and its potential role in pain relief.
The most abundant of all the phytocannabinoids - at least in terms of percentage of total content percentage in the majority of cannabis cultivars – is THC. This is the psychoactive compound responsible for producing the 'high' associated with recreational cannabis use, and this effect can also be explained by its interaction with the ECS.
THC has been shown to have a strong binding affinity for CB1 receptors. CB1 receptors are, for the most part, found in the brain and central nervous system, so when THC binds to these receptors it triggers changes in neurotransmitter release. This can produce a variety of effects – both therapeutic and psychoactive – depending on the dose administered, the method of administration, as well as the patient's own unique response to THC.
THC has been shown, through a variety of clinical studies, to have enormous potential in the management and relief of pain. These studies have indicated that it may be helpful in treating inflammatory and neuropathic pain specifically, with some evidence suggesting its potential to help manage chronic pain as well.
This 2010 randomised control study, titled "Smoked cannabis for chronic neuropathic pain", came to some pretty conclusive results regarding the role of THC in pain relief. While not huge in scale, with only twenty-three participants, this study suggested that smoked cannabis did indeed reduce neuropathic pain significantly. The paper concludes:
"A single inhalation of 25 mg of 9.4% tetrahydrocannabinol (THC) herbal cannabis three times daily for five days reduced the intensity of pain, improved sleep and was well tolerated"
One comprehensive review, A comprehensive analysis of four studies, investigated the effectiveness of cannabis in managing both surgical and non-surgical back pain. The studies employed different forms of cannabis, including THC-dominant dried flower, synthetic THC (dronabinol), and a synthetic THC analogue (Nabilone). The review found that:
“In all articles, cannabis was shown to be effective to treat back pain with an acceptable side effect profile”
THC administration for chronic pain has been extensively studied and has consistently shown promising results in decreasing the need for opioid medications. In fact, one study highlighted a remarkable 64% reduction in opioid use among chronic pain patients who incorporated medical cannabis into their treatment regimen.
This reduction may very well help to mitigate the potential for harmful and even fatal side effects associated with opioids. The significance of medicinal cannabis as a viable treatment option for chronic pain relief has therefore grown exponentially, offering a safer and more sustainable alternative for patients in need.
CBD and pain relief
Although CBD and THC share the exact same chemical formula, their chemical structure is slightly different, which results in vastly different effects on the body. This is because unlike THC, CBD does not have the same ability to directly bind to the CB1 receptor, which is thought to be the reason it is a non-intoxicating compound.
However, CBD does interact with the body in many other ways. It can bind in weak interaction with the CB2 receptor, while also influencing how endocannabinoids and THC interact with the CB1 receptor. CBD has also been shown to inhibit the enzyme responsible for breaking down anandamide, one of the body’s own naturally occurring endocannabinoids. It is also able to modulate the serotonin system, and the TRPV1 signalling pathways.
So, what does all of this mean for pain relief?
A lot, actually.
Let's look at the TRPV1 signalling pathways first. TRPV1 receptors respond to a variety of stimuli, including temperature, pain, and inflammation. The endocannabinoids produced by the ECS modulate TRPV1 activity, affecting how it reacts to these different stimuli. When CBD binds to TRPV1 receptors, it can help regulate their activity, resulting in reduced sensitivity to painful stimuli and a decrease in inflammatory markers.
In real world studies, CBD has been shown to have a positive impact on reducing pain, with some studies suggesting that it may be helpful for conditions such as fibromyalgia and rheumatoid arthritis.
This paper, from 2015, looked at how transdermal (applied to the skin) CBD can affect chronic arthritic pain. While no human trials were conducted with this study, the results suggested that transdermal CBD could help reduce inflammation and pain-related behaviours in arthritic rats, without evident side effects.
Another study looked at how CBD may be an effective pain-relieving option for patients that had just undergone kidney transplant surgery. The dosage levels started at 50 mg and were slowly increased to 150 mg over a three-week period. The study only included 7 participants, but found that:
"Two patients had total pain improvement, four had a partial response in the first 15 days, and in 1 there was no change" and "CBD was well-tolerated, and there were no severe adverse effects."
In one of the more recent open-label studies looking at how CBD can help with chronic pain management, researchers came to some promising conclusions. They noted a significant reduction in pain intensity among the participants who ingested CBD, as well as improved sleep and minimal side effects. The authors finish the paper with:
"CBD has shown potential as a treatment for chronic pain and certain forms of epilepsy, improving quality of life and providing analgesia" and that "CBD may increase the bioavailability of endogenous mediators of pain (i.e. serotonin) and exogenous analgesics (i.e. THC)"
Are cannabinoids free from side effects?
Definitely not. As with all medications, cannabinoids can cause unwanted side effects.
As CBD and THC have different pathways of action and affect the body in different ways, it's important to know which side effects may be associated with each.
THC is known for its psychoactive/intoxicating properties. This means that it does come with some risk of dependence occurring, but when the dose is managed this risk can be minimised. Common side effects of THC include:
- Dry mouth/increased thirst
- Dizziness
- Lowered blood pressure
- Red eyes
- Increased heart rate
- Paranoia or panic
CBD, on the other hand, is non-intoxicating and so comes with zero risk of addiction. The potential side effects of CBD are much milder and include:
- Dry mouth
- Lowered blood pressure
- Drowsiness or fatigue
- Gastrointestinal discomfort
Is there a risk of overdose?
Generally, no. Unlike opioids or certain other medications, it is not possible to overdose on cannabis or cannabinoids. While heavy doses of THC can produce adverse effects, such as paranoia or anxiety, they typically dissipate within an hour or two and are not life-threatening.
However, it is still important to take cannabinoids responsibly and be aware of the potential side effects that may occur.
All of this simply goes to show just how important it is to seek the guidance of a doctor that is experienced in prescribing cannabis-based medical products for your specific healthcare needs before making any changes to your current treatment regime.
Comparing cannabinoids and convention pain medication options
| Medication |
Efficacy for Pain |
Side Effects |
Risk of Dependence/Addiction |
Risk of Overdose |
| CBD |
Moderate |
Dry mouth, diarrhoea, reduced appetite, drowsiness, fatigue |
Low |
Low |
| THC |
Moderate to High |
Dizziness, sedation, cognitive impairment, psychological effects, increased heart rate
|
Low when prescribed and the dose is controlled, although dependence can occur |
Low |
| Opioids (e.g. Morphine, Oxycodone) |
High |
Nausea, constipation, sedation, respiratory depression, addiction, overdose |
Moderate to high |
High |
| NSAIDs (e.g. Ibuprofen, Naproxen) |
Moderate |
Gastrointestinal upset, renal dysfunction, cardiovascular events |
Low |
Low |
| Antidepressants/Anticonvulsants (e.g. Gabapentin, Amitriptyline) |
Moderate |
Sedation, cognitive impairment, dry mouth, blurred vision |
Low |
Low |
Cannabinoids for pain – the wrap-up
Once again, cannabinoids (specifically THC and CBD) should never be applied as a replacement for your current medications. The ever-growing body of evidence suggests that, when taken correctly and in the right dosage, they have a good safety profile and can offer complementary benefits to reduce inflammation, alleviate pain, and improve quality of life for those suffering from chronic or persistent pain.
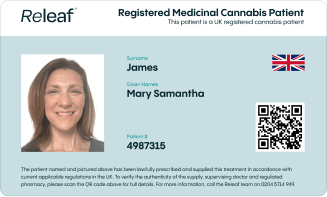
Do not allow the negative perception sometimes associated with medical cannabis to deter you or your loved ones from accessing the best treatment options for your individual healthcare requirements. Releaf provides tailored monthly packages, specialist consultations for medical cannabis, and a unique medical cannabis card for protection, all based on your medical cannabis prescription.